LL Part 23: How likely was it that the Neonates at CoCH would Survive?
Using whole-of-country maternal data for the United Kingdom
Following on from our last post on the Lucy Letby Trial Here
Summary:
The Countess of Chester Hospital babies that Lucy Letby was accused of harming had a very high likelihood of stillbirth or neonatal death within the first 7 days of their life.
We observe known values for each of five babies on a Bayesian network model and find that the minimum probability for mortality for each baby was:
Baby A - 1 in 4 (24.3%)
Baby C - 1 in 5 (18.2%)
Baby D - 1 in 166 (0.6%)
Baby E - 1 in 10 to 1 in 2.6 (9.7% - 38%)
Baby K - 1 in 2.3 to 1 in 2 (43.7 - 49%)
The background rate of stillbirth and neonatal mortality in England and Wales during 2021 was 1 in 160 (0.6%) which means all except Baby D, who was right on the average, had an extremely elevated risk of dying.
Introduction
As many of my readers will doubtless know, a jury took what I believe was just shy of three and a half hours to convict Lucy Letby of the attempted murder of Baby K.
I would like to correct one mistake I personally have made in the last couple of days when discussing the trial for Baby K. The charge for Baby K was laid at Letby’s feet during the original trial however, the jury were unable to reach a verdict at that time. That, in fact, means that this was a retrial. I have been having discussions with other legally minded people over the last week with respect of when (or if) Letby would be prosecuted for the neonate that Justice Goss had the prosecution remove from the docket of the original trial, and as a result got the two confused in my mind. That is my mistake and comes about from doing a lot of research on the case during the last week with little sleep. It does nothing to change the outcome but I at least wanted to recognise the contextual error on my part before moving on.
Most predictive models in medicine, and especially in maternity, use observations of a small number of factors such as signs and symptoms and test results that are related to a single health issue - such as predicting whether the mother may develop gestational diabetes (GDM) during her pregnancy by using her ethnicity, BMI and HbA1c, or preeclampsia by using her blood pressure, previous history of preeclampsia, BMI and maternal age.
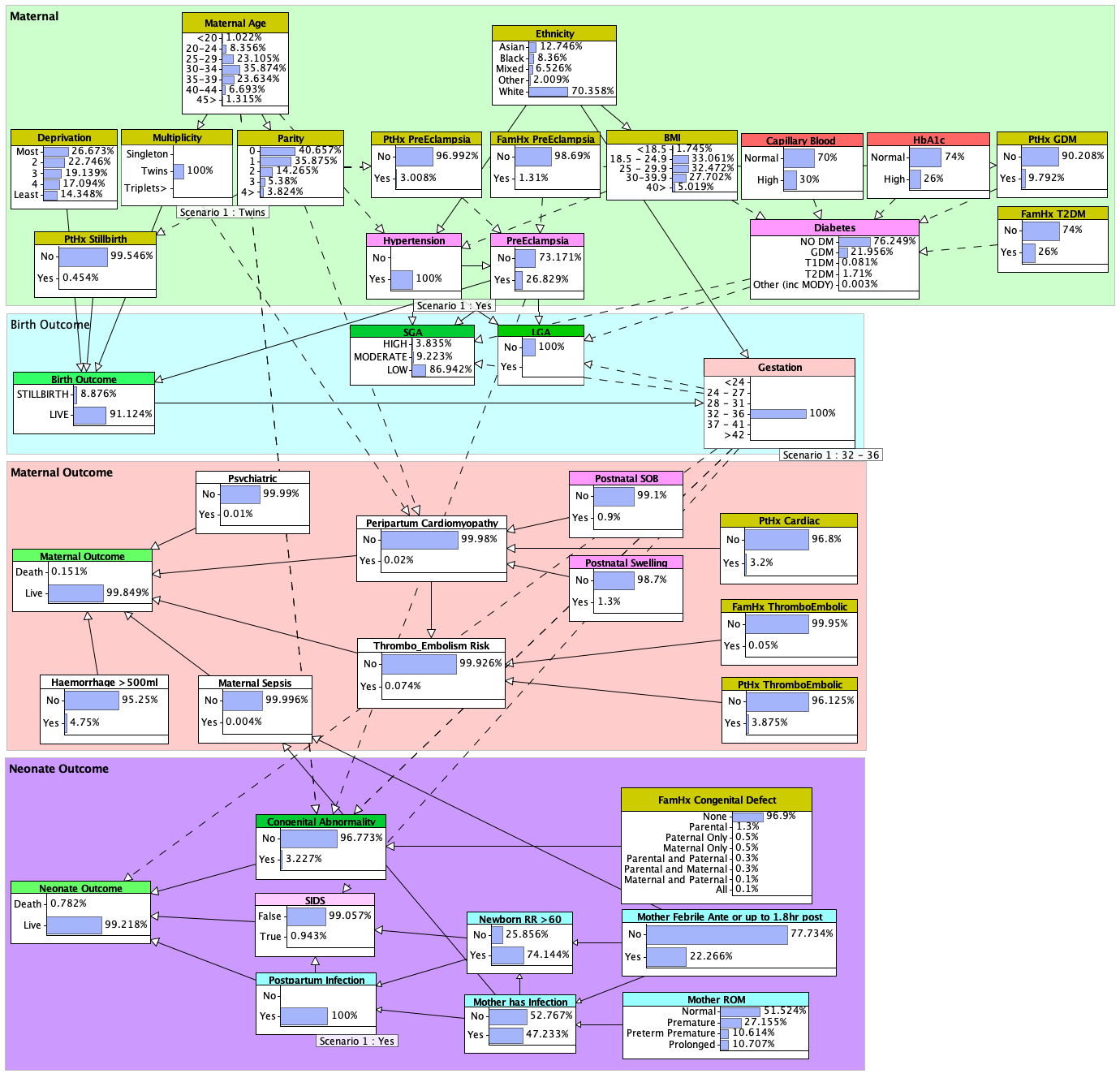
I recently completed some work developing the first version of a large Bayesian network model that looks at the basic relationships between a much broader range of factors in order to make predictions about several important outcomes in maternal health: the birth outcome, the maternal outcome, and the neonate outcome.
While this is an early version of the model and there are more factors for which we are already incorporating data for release of a second even larger version, we have already released a large preprint describing the process and data used to construct the model and our validation methodology (here), and a peer reviewed academic paper and conference proceeding (here). I will repeat a few of the salient facts here that are necessary to your understanding of the analysis and results I will describe with respect to some of the babies Lucy Letby was prosecuted for harming.
Training Data
The data for the model presented in this work were derived from the following publicly available privacy-preserving statistical sources:
The United Kingdom (UK) Office for National Statistics (ONS):
• Birth Characteristics 2021 dataset [27]
• Child and Infant Mortality 2021 dataset
• Preconception health among migrant women in England 2019-2021 datasetMothers and Babies: Reducing Risk through Audits and Confidential Enquiries across the UK (MBRRACE-UK)
• MBRRACE-UK Perinatal Mortality Surveillance: UK Perinatal Deaths for births from January to December 2021Public Health England (PHE) National Congenital Abnormality and Rare Disease Registration Service (NCARDRS)
• NCARDRS Congenital abnormality statistics: Annual data 2021 dataset [51]
These sources describe a broad range of risk factors and their incidence for the following events that occurred in England
and Wales during 2021:
624,828 pregnancies (including 8,470 multiparous1 pregnancies)
624,162 live births
2,579 stillbirths
1,353 neonatal deaths under 7 days
1,715 neonatal deaths under 28 days
608 post-neonatal deaths 28 days or over
312 post-neonatal deaths between 4 weeks and 3 months
160 post-neonatal deaths between 3 and 6 months, and
136 post-neonatal deaths between 6 months and 1 year
Additional evidence for establishing incidence and causal relationships between risk factors and symptoms were derived from clinical practice guidelines and academic studies of pregnancy and pregnancy outcomes published between 2019 and 2022. Emphasis was given to those studies that described data collected in 2021 from UK populations.
For the purposes of the study I am doing here regarding the CoCH neonates, I have limited the data used in the neonatal outcome node to deaths that occured within the first 7 days. In the UK during 2021 there were 3,932 stillbirth and neonatal deaths within the first 7 days - roughly 0.63% of pregnancies or 1 in 160 babies.
How We Use The Model
The process for using this model is quite simple. On any node that we can identify some relevant information from the trial transcripts and evidence, we observe that value and run the model. The model will return results for the other nodes, updated based on the observation/s we have entered.
Focusing briefly on just the Maternal and Birth Outcome panels and without making any observations about a particular mother, we can see what are called the priors - that is, the background values for each node based on the knowledge learned from the training data. Remember that the training data was every one of the nearly 625,000 pregnancies that occured in the UK during 2021.
We can see that the vast majority of women in the UK (90.59%) delivered within the period that midwives and obstetricians call term - that is, the expected window from 37 - 41 weeks gestation. Prematurity occurs for a small group of pregnancies, but around 7% is hardly rare. However, extreme prematurity, that is - before 28 weeks, is rare. Extreme prematurity occurs in less than half a percent (0.475%) of all UK pregnanices. We can also see that the age of the mother (maternal age) falls within a neat bell curve, with the peak at 30-34 years of age. Finally, the most important thing we can see is that the typical stillbirth rate in the UK is just under 0.5% - meaning stillbirth typically occurs in 1 in 200 pregnancies.
Note: Where a pregnancy is lost very early, typically in the first trimester but based on most guidelines, somewhere before 21-24 weeks gestation, we call this a miscarriage. The miscarriage rate is somewhat higher in the UK than the stillbirth rate. Miscarriages are not included in the data that was used to train this model.
Note 2: Some mortality that has been recorded in the national statistics as stillbirth is actually early neonatal death. Hospitals have been doing this to avoid the additional scruitiny and neonatal mortality and coronial review required when a live baby dies in the hospital. A review is currently underway to ascertain the scale of this issue but one news article described how a brief examination of records at one exemplar hospital quickly identified six live-born neonates, most having died within minutes or hours after birth but including one who was an incredible five days old, that had all been registered as stillbirth deaths. Played out across the entire NHS, and given that very few deaths are actually referred for coronial investigation each year, there could be many hundreds or more each year being incorrectly categorised and recorded in this way. For this reason the Birth Outcome node actually describes the likelihood of both stillbirth or neonatal death up to and within the first 6-12 hours which, in many cases, includes a stay in a neonatal unit.
In order to arrive at a total describing the probability of a negative (death) outcome, we will add the stillbirth value from the Birth Outcome node with neonatal death value from the Neonatal Outcome (within 7 days, remember!). This approach will be used in all of the CoCH examples that follow.
For example: if we were to observe a white mother (Ethnicity: White) who has had two previous pregnancies (Parity: 2 - meaning she is now on her third pregnancy) and her first pregnancy ended in a stillbirth (PtHx Stillbirth: Yes). She has just arrived at the maternity unit and goes into irreversible labour prematurely at 28 weeks (Gestation: 28-31). We can see that the probability of a live birth (survival) for this pregnancy is 50.97% (meaning the likelihood for this pregnancy to end in either a stillbirth or neonatal death in the first 6-12 hours is a very high 49.02%).
It takes nearly 40 hours from when her waters break to delivery (Mother ROM: Prolonged). She was observed to have an increasing fever in the hours before delivery (Mother Febrile: Yes) and both she and her neonate are being treated for a suspected staph infection (Mother has infection: Yes, Postpartum Infection: Yes). Her neonate is very fortunate and survives childbirth and is immediately transported to the NICU.
These additional observations have further increased the likelihood of death for this neonate by 1.104%, making the overall probability for a negative (death) outcome 50.124% (49.02 + 1.104). The probability that this mother’s child survives his first 7 days of life (100 - 50.124) is unfortunately slightly less than half (49.876%).
Some Countess of Chester Babies
Baby A
Letby was found guilty of the allegation that she injected air directly into the neonate’s blood stream. We have the following observations for Baby A:
Baby A was the second of a set of twins (Multiplicity: Twins)
Baby A’s mother had or was suspected to have preeclampsia (Preeclampsia: Yes)
Baby A was treated for suspected sepsis (Postpartum Infection: Yes)
Baby A was 6 weeks premature (34 weeks gestation)
The overall probability for neonatal mortality for Baby A within the first 7 days of life was 24.3% (23.498 + 0.771). Absent other observations about the mother or her pregnancy, there was already a 1 in 4 probability that Baby A would not survive his first 7 days of life.
Baby C
Letby was found guilty of the allegation that she injected air into his stomach. We can make the following observations on the model for Baby C based on evidence and testimony:
Baby C was a single pregnancy (Multiplicity: Singleton)
Baby C was 7 weeks premature (Gestation: 32-36 Weeks)
Baby C’s mother’s waters had broken (Mother ROM: Preterm Premature)
Baby C was Small for Gestational Age and was only around 800g at birth (SGA: High)
Baby C’s mother had gestational hypertension (Hypertension: Yes)
Baby C was treated for suspected sepsis (Postpartum Infection: Yes)
Absent other observations, the overall probability for neonatal mortality for Baby C within the first 7 days of life was 18.2% (17.327 + 0.833) or 1 in 5.
Baby D
Letby was found guilty of the allegation that she injected air directly into the bloodstream of Baby D. For Baby D we can observe the following:
Baby D’s mother’s waters broke premature, and more than 50 hours before Baby D was delivered (Mother ROM: Prolonged)
Baby D was a single pregnancy (Multiplicity: Singleton)
Baby D was meant to receive antibiotics at birth but did not. She was later diagnosed with suspected sepsis and signs of a lung infection were observed on x-ray (Postpartum Infection: Yes)
Baby D had transient tachypnoea of the newborn (TTN) causing her to have periods of very rapid breathing (Newborn RR > 60: Yes)
Baby D was a term Baby (Gestation: 37-41 Weeks)
Baby D was the least likely baby to die. Absent other observations, the overall probability for neonatal mortality for Baby D within the first 7 days of life was 0.6% (0.132 + 0.465) or 1 in 166. Baby D’s death was not statistically significant however, as the likelihood for mortality was right at the background rate for stillbirth and neonatal deaths in the first 7 days in the UK.
Baby E
Letby was found guilty of the allegation that she injected air directly into the bloodstream of Baby E. For Baby E we can observe the following:
Baby E was delivered 7 weeks premature (Gestation: 32-36 weeks)
Baby E was one of a set of twins: (Multiplicity: Twins)
Baby E was suspected of having sepsis and NEC (Postpartum Infection: Yes)
Baby E’s mother likely had gestational hypertension that caused her to go into premature labour (Hypertension: Yes)
Absent other observations, the overall probability for neonatal mortality for Baby E within the first 7 days of life was 9.7% (8.867 + 0.782) or 1 in 10.
Baby E had issues with hyperglycaemia and insulin regulation that could have been congenital, birth-related, or related to the sepsis infection he quite clearly had. The impact of these factors cannot be incorporated into the current model. Baby E also had a further complication in that he was what is known as an assisted reproduction baby - his mother had IVF in order to concieve Baby E and his brother, Baby F. Assisted reproduction is associated with an increased risk for neonatal death. Not only are mothers of assisted reproduction twins at an increased risk of gestational hypertension and gestational diabetes compared to their non-assisted reproduction peers, live-born assisted reproduction twins are at an additional 28% risk of neonatal death compared to non-assisted reproduction twins.
If we factor in this additional 28% we find that the risk of mortality for Baby E was closer to 38%, or 1 in 2.6.
Baby K
Turning to baby K we have only three observations available to us:
Baby K was 24 weeks 6 days gestation when her mother went into labour. Baby K was delivered at 25 weeks 2 days (Gestation: 24-27 weeks).
Baby K’s mother went into labour preterm, and her membranes ruptured (her water broke) in the hours before delivery. My midwifery reviewer tells me that this is classed as a preterm-premature (Mother ROM: Preterm-Premature).
We are not told whether Baby K’s mother had an infection - however, given that she was in labour for two days it would have been common to administer prophylactic antibiotics to her. All we do know is that Baby K was given prophylactic antibiotics for a suspected infection and that a culture test, which are notoriously inaccurate, suggested no infection. It is likely Baby K had an infection (Postpartum Infection: Yes).
Absent other observations, the overall probability for neonatal mortality for Baby K within the first 7 days of life was 43.7% (42.614 + 1.1). If the mother was of white british or european ethnicity, this increases the probability for mortality to 46.8% (45.652 + 1.099) and further, if it was also later found that the amniocentisis screening that only looked for common conditions like Downs Syndrome actually missed the suspected congenital abnormality, this would further increase the probability for mortality to 49% (42.496 + 6.505). Even worse: If Baby K’s mother had delivered prematurely as a result of preeclampsia2, the probability for mortality at such an early gestation increases sharply to 91% (89.945 + 1.051) - making Baby K’s overall survival very unlikely.
While it is emotionally devastating for the parents, based on current clinical data and knowledge and absent additional information about the mother and her pregnancy, any common sense clinical assessment should find that Baby K had somewhere between 43-49% probability (or 1 in 2) for mortality in the first 7 days from birth.
Conclusion
What we can see from this analysis is that all but one of the Countess of Chester Hospital babies that Lucy Letby allegedly harmed had a significantly high probability of stillbirth or neonatal mortality even just within the first 7 days of life. Further, the probability for that one exception, Baby D, was actually right on the national average for pregnancies like him.
The next part in my series on Lucy Letby can be found here.
Multiparous means pregnancies where there was more than one baby - i.e. twins, triplets and so on.
Preeclampsia is a type of high blood pressure that affects pregnant women and is one of the more common conditions of pregnancy. Depending on country and ethnicity, preeclampsia can occur in 1 in 25 pregnancies (4%) or more, and while it can occur from 20 weeks gestation, most cases are seen from 24 weeks gestation onwards.











If that doesn't look like 'reasonable doubt' then I'm, erm, I don't know, the pope, maybe. Certainly not someone who did actually get a B grade in A-level maths which involved a fair amount of stats & prob, and can follow your reasoning.
One larger probability comparison I would love to see is with other comparable NICUs. Statistically speaking, I mean, given that every baby in an NICU has an elevated probability of dying, what is the average for a level 2 NICU mortality cluster. Likewise, what would be the probability of any randomly selected NICU nurse being associated with a cluster of deaths. I would imagine we're talking about 'standard deviations' here. Given the number of NICUs, and over a given number of years, I would imagine the percentage chance is 99.9% or something. And the more years which pass the tendency towards 100% increases, until 'it happens'. Thus, what really determines whether a nurse gets accused (let alone prosecuted) is the personality of the people around her, in particular the specialists. I would not be surprised if Lucy wasn't the only nurse statistically associated with such a cluster, just that she happened to be the only one surrounded by sociopaths, including a 'TV Doctor' with a sunk cost fallacy. If you get my meaning.
Anyhow, I think the point here is that serious monitoring, psychologically speaking, of the personality types in high risk environments like an NICU needs to be a matter of course. That kind of monitoring could've prevented this entire miscarriage of justice.
You have done amazing work here, by the way. I'm not surprised you haven't had much sleep! And I do hope that all of this can get to whichever uncorrupted future defence team LL might have, and thus lead to a total acquittal. And sooner, rather than later.
I would find it really helpful if you could note on past discussion of particular babies what the relevant trial verdict was.
Thank you for this article. I was aware of the general pattern and principles but very helpful to see the risks quantified. Given the significant increase in high risk babies on the change to level 2, the consultants should have expected the number of deaths to increase. Are they bad at maths/lacking numeracy? Another possibility is that they tried to discredit a nurse whom they knew would be a whistleblower when there were problems? Probably hoping she would move hospitals rather than prison for life.