LL Part 18: What happened to Baby F?
Insulin, Dextrose, Two kinds of Antibiotics, and... yep... Sepsis
Following on from our previous article on the Lucy Letby Trial here.
The prosecution alleged Lucy Letby attempted to murder Child F by insulin poisoning on August 5.
July 29, 2015
The mother gave birth to twins (Babies E and F) prematurely by emergency caesarean section (EMCS) and believed they were in ‘good condition for the gestation they were in’ at birth. Mother says she does not remember any specific conversation about insulin production for the twins, but remembers it being mentioned, and that it was 'normal' for premature babies.
In fact, Baby F was in such ‘good condition for the gestation’ that he required resuscitation at birth, and very shortly after had to be intubated, ventilated and given surfactant medication to aid in preventing alveolar collapse and to reduce the risk of neonatal respiratory distress syndrome (NRDS).
Baby F was 1.434kg on delivery, but over his first 1-2 days dropped approximately 10% (140 grams) to 1.296kg. His blood glucose reading taken shortly after birth was 2.7mmol. A second blood glucose reading taken a few hours later was 1.9mmol. Baby F had been struggling to breath and so as a result was started on a 10% glucose infusion.
July 30, 2015
Baby F’s mother wasn’t able to cuddle him as he was on CPAP during the entire day.
Baby F’s blood glucose reading was recorded as 15.1 at 9:57pm.
July 31, 2015
A blood glucose reading 2.5 hours later at 12:22am showed Baby F still had elevated blood glucose at 13.9mmol. He was prescribed insulin to correct it, which was administered at 3:40am.
Baby F’s blood glucose was taken again at 4:41am and found to be 8.7mmol. This was taken to mean he had ‘responded well’ to the insulin infusion.
The insulin infusion was stopped after nearly three hours at 6:20am.
At the same time Baby F’s endotracheal (ET) breathing tube was removed and he was given CPAP breathing support.
August 1, 2015
Letby was designated nurse for Baby F on Night Shift.
August 2, 2015
Letby was again the designated nurse for Baby F on Night Shift.
The day shift nurses had attempted to withdraw CPAP from Baby F during the morning but this had led to several desaturation events and necessitated resumption of full CPAP supported breathing.
Dr Gibbs recorded during ward rounds that Baby F was recovering from respiratory distress syndrome, was being treated for ‘suspected sepsis’, had ‘some jaundice’ and had lost 10% body weight since birth. He also noted that Baby F’s blood sugar levels were still high, peaking at 10mmol. He noted that another doctor had suggested Baby F had a heart murmur, but that he had not heard it upon his own examination. The management plan for Baby F included ‘standard TPN’ administration along with nasogastric feeds of expressed breast milk (EBM).
Dr Gibbs testified that Baby F also had recurrent ‘intermittent desaturations’ - periods when his oxygen saturation level would spontaneously drop and self-correct. He also said that he might not have heard the heart murmur because the CPAP machine was on at the time he examined Baby F.
August 3, 2015
At the end of her night shift, Nurse Taylor handed over to the unnamed nurse for the day shift at around 8:00am. The unnamed nurse was the designated nurse for both Babies E and F. Baby F at this time was on CPAP but was not considered to be stable.
August 4, 2015
At 1:24am care was withdrawn for Baby F’s brother, Baby E, and he was pronounced deceased.
At 5:00pm a nursing note recorded that the parents had asked for Baby F to be transferred to another hospital. The doctors told them that transport was ‘unavailable’ due to ‘another emergency’.
When night shift began at 8:00pm the unnamed nurse was designated nurse for Baby F, and Lucy Letby was designated nurse for another premature neonate in the same room. This night shift is one where there was almost a 2-to-1 ratio of babies to nurses - seven neonates being cared for by four nurses - because the fifth nurse, the shift lead Nurse Simcock, would normally not be allocated as a designated nurse to any of the neonates. Given that Lucy and the unnamed nurse were both in Room 2 with the two babies requiring the highest acuity intensive care, that left five other neonates in three other rooms being cared for by the two remaining nurses, with all nurses being able to call on the assistance of Nurse Simcock.
Baby F’s blood gasses were recorded at 11:32pm, showing his blood glucose level at that time was 5.5mmol.
Dr Beech reviewed Baby F during the day shift. She reported that Baby F had been on OptiFlow ‘on air’ (i.e.: without supplemental oxygen) since 3:30am. OptiFlow is a less invasive positive pressure nasal high flow (NHF) assisted breathing device using nasal prongs rather than a CPAP mask.
Dr Beech also noted that Baby F had ‘suspected sepsis’ and noted raised urea and creatinine levels and low level jaundice. She reported that Baby F had started on ‘establishing feeds’, was awaiting a genetic test for Trisomy 21 (Downs Syndrome), and that his hyperglycaemia was ‘resolved’. She prescribed what she described in evidence as ‘a standard list of medication’. Her management plan for Baby F included that he should complete a 7 day course of antibiotics (for the sepsis), that if he continued to tolerate feeds the nursing staff should continue to increase them, that the genetic tests should be ‘chased’, and that the full head-to-toe check should be completed at some future time.
At 5:40pm Dr Beech made a note that she was ‘asked at handover to prescribe 150ml/kg/day of 15% Dextrose over 24 hours with 5ml/kg/day in it’ and ‘to stop TPN, check urinary sodium, cortisol and insulin.’ The urinary tests all returned ‘no unusual readings’.
At 7:00pm Dr Beech prescribed Baby F a 15% Dextrose with 0.9% Saline infusion.
August 5, 2015
At 12:25am Letby signed to record that a 48 hour Total Parenteral Nutrition (TPN) infusion had finished.
A new TPN mixture was prescribed that called for a higher concentration of Babiven (70ml/kg) with the addition of Intralipid (lipids) and 10% Dextrose solution that had not been in the just completed infusion. The new Babiven was recorded as started at 12:25am, while the Intralipid was recorded as commenced at 3:10am. Lucy co-signed for the Babiven but was not a co-signer, and was most likely not involved in, the Intralipid administration. There were two separate orders written for the change of TPN, with the first having been crossed out. Dr Beech testified that she had written the first (crossed out) order, and that another colleague had written the amended (corrected) order.
The prosecution alleged that Baby F first started to decline after the new Babiven TPN was commenced at 12:25am. They supported this claim initially by showing Baby F’s fluid chart that recorded NGT aspirates and vomit at 1:00am with four plus signs (++++) beside it and a retrospective nursing note written for 1:00am reported a large milky vomit. That note also recorded that Baby F’s heart rate was tachycardic at 200-210 beats per minute, with elevated respiration rate of 65-80 breaths per minute and O2 saturation at >96%. It says Baby F ‘became quieter than usual’ and that his abdomen was soft and not distended, that he was ‘slightly jaundiced’ but there was no loss in colour. It concluded by saying that Dr Harkness was going to review Baby F.
Baby F’s observations recorded by the unnamed nurse at 1:15am showed that Baby F’s heart and respiratory rates were both elevated into the alert (yellow) area on the chart.
At 1:30am Dr Harkness telephoned Dr Gibbs with concerns over the fact that as the nasogastric feeds had been increased, Baby F had ‘multiple small milky vomits and 9ml of milk aspirate’, and a heart rate above 200.’ Even on reviewing this evidence and admitting that heart rates over 200 were ‘very unusual’, Dr Gibbs in testimony still maintained that Baby F was “a health baby.” Dr Harkness had assumed at the time that these changes were indicative of and due to infection but Dr Gibbs, on reflection with refreshed memory while testifying, sought to re-characterise them as ‘very rapid, even for infection.’ He argued that it was not an infection because there would normally have been signs of deterioration beforehand which, if you reflect on what you have already read in this article, are clearly present. Their plan at the time was to screen Baby F for infection and to start a second line for a different course of antibiotics. In spite of the fact that Baby F had been continuously receiving fluids via TPN, IV and nasogastric routes - dehydration was also considered as an alternate cause to infection. Additional fluids and saline were to be administered as a result.
At this point Baby F’s nasogastric feeds were ceased.
A blood gas reading recorded at 1:54am showed Baby F’s blood glucose to be 0.8mmol. As a result of this observation, at 2:05am Baby F was given an intravenous infusion of 10% Dextrose solution at 2:05am along with several other medications. Blood tests for Baby F were ordered by doctors at 2:15am and 2:17am, which were collected at 2:33am and 2:45am respectively.
Baby F’s blood glucose was checked again at 2:55am and found to be 2.3mmol.
Baby F was given a 0.9% saline infusion at 3:35am, and at 3:50am a further 10% Dextrose solution was administered intravenously. At 4:02am Baby F’s blood glucose was measured again and found to be 1.9. A further infusion of 10% Dextrose was given at 4:25am and his blood glucose was found to be 2.9mmol at 5:00am. Lucy Letby was the author of the 5am blood glucose level.
Nurse Tomlins was the designated nurse for Baby F during the day shift on August 5th.
Baby F’s blood glucose was charted during the day shift as 1.7 at 8:00am (note that Letby texted a colleague that it was 1.8 at 8:00am), 1.3 at 10:00am, 1.4 at 11:46am, 2.4 at 12:00pm, 1.9 at 2:00pm, 1.3 at 3:01pm, 1.9 at 4:00pm, 1.3 at 5:56pm and 1.9 at 6:00pm.
A medical note by Dr Gibbs at 8:30am recorded that Baby F’s blood glucose was 1.7mmol despite administration of glucose and that he believed the elevation in heart rate was natural and due to stress. At the same time he also recorded that Baby F had signs of decreased circulation, which he testified was likely due to ‘stress, dehydration or an infection’. He still queried sepsis but testified that he discounted this and NEC due to the lack of signs for it on the blood gas results. He also testified that his query of sepsis in the notes was to remind himself to consult the new ‘consultant of the week’ to order a possible abdominal x-ray to look for signs of NEC.
The unnamed nurse administered a bolus intravenous infusion of glucose to Baby F at 8:30am.
At 10:00am there were issues with Baby F’s intravenous cannula and this had to be re-sited.
At 11:00am Dr Gibbs recorded that the TPN, which included the 10% Dextrose, was ‘off’ as the line had ‘tissued’.
It was noted that the long line had tissued and as a result Baby F’s thigh was ‘swollen’. It was thought at the time that the tissued long line may actually have been the cause of Baby F’s hypoglycaemia during the day.
A new long line was inserted at 12:00pm.
The unnamed nurse administered a bolus intravenous infusion of glucose to Baby F at 3:15pm.
The blood test for insulin that was sent to Royal Liverpool Hospital (RLH) was reported as having been drawn at 5:56pm.
At 7:00pm a new TPN fluid order was made by Dr Gibbs and commenced - ceasing the TPN, Lipid and 10% Dextrose that he had been receiving and replacing it with a 15% Dextrose and 0.9% saline infusion. The unnamed nurse signed for the administration of this dose.
At 8:00pm the same unnamed nurse who had cared for Baby F on the previous nights returned and was designated nurse for Baby F again. She messaged Letby that Baby F was ‘more stable’ with a heart rate of 160-170 beats per minute.
At 9:17pm Baby F’s blood glucose was measured at 4.1mmol.
August 6, 2015
At 1:30am Baby F’s blood glucose had risen to 9.9mmol, and it remained at this level when re-tested at 2:00am.
At 2:00am Baby F was given another infusion of 15% Dextrose that was witnessed and co-signed by the unnamed nurse.
Discussion
I spent quite a while trying to find any reporting of Baby F being prescribed and administered insulin in the mainstream reporting on the case. The only mention I found was in the Chester Standard’s ‘blow by blow’ reporting of the trial on the 22nd of November. However, even the journalists at the Chester Standard felt the need to editorialise what was said in court wherein they described it as ‘a tiny dose’. While a dose of 0.2units/kg/hr via a syringe driver might sound to adults like a tiny dose, for a neonate it is actually quite a significant dose that would see the premature 1kg baby potentially receiving almost 5 units of insulin over a 24 hour period. The prosecution very carefully led with this evidence but very little attention was drawn back to it or the importance of this evidence during the remaining testimony on Baby F.
All other reports avoided mentioning that Baby F had ever been prescribed or legitimately administered insulin, preferring instead to focus on the allegedly high level or the absence of a similar level of c-peptides and drawing the reader’s attention to Dewi Evans’ claims that this could only be because Baby F was administered the insulin via a doped TPN feed (here, here and here). Other papers told the public that only two nurses were on shift (Letby and Simcock) in spite of the fact that evidence adduced in court showed there were actually five nurses on duty and Simcock was the shift leader on the night and not the other ‘unnamed’ nurse present in Room 2 during most of the shift (here). It seems the mainstream media played pretty fast and loose with the truth and only told you what you needed to hear in order to believe the prosecution assertion that the only way insulin could ever be found in Baby F’s bloodstream was if Lucy had poisoned Baby F.
The blood test for insulin that was sent to Royal Liverpool Hospital (RLH) was reported as being drawn at 5:56pm. You will note from the charted blood glucose values that Baby F’s blood glucose was 1.9 at 4:00pm and 1.9 again at 6:00pm, but was only 1.3 at 5:56pm when the blood test was drawn. We should ask what happened either between the 4:00pm test but before the draw at 5:56pm, or in the few minutes after the 5:56pm blood draw and the 6:00pm re-test to cause the drop to 1.3, or the return to the previous value of 1.9 almost immediately after? Further, why was Baby F’s blood glucose tested a second time only 4 minutes after the test that was done on the blood draw? Did two tests that resulted in two different blood glucose readings actually occur or is this another anomaly either in the health records of the CoCH neonatal unit or in the testimony and medical evidence presented by the prosecution? Professor Hindmarsh explained away this discrepancy as being nothing more than an acceptable difference of up to 0.8mmol between measurements.
While many of the clinical notes on the afternoon of August 4 were made by Dr Beech, several times she testified that she ‘could not recall’ making the note, or could not recall whether or not Baby F had received particular treatments such as the additional Dextrose doses. It was also Dr Beech who testified regarding the results of the blood test she took that was sent to RLH, and that insulin and c-peptide levels are ‘expected to be similar’. It was her testimony that established that Baby F’s insulin reading was 4,657 and his c-peptide level was 169.
It was interesting that after having Dr Beech testify as to collecting the blood test that was sent to RLH and its results, the prosecution placed another unnamed doctor on the stand who, after telling the court she had had absolutely no involvement in the care of Baby F whatsoever, was then asked to read the notes of yet another unnamed junior doctor. Why did the prosecution not simply get Dr Beech to read that junior doctor’s notes? Why did they feel the need to bring in this unnamed paediatric doctor to simply read a different doctor’s clinical notes? Did Dr Beech refuse to read them? And, if so, why? Also, why is it that this unnamed doctor was the one they used to deliver the statement ‘there are some medical conditions where a low blood sugar reading would also mean a high insulin reading, but the low insulin c-peptide reading meant that those conditions could be ruled out’. Would this not be evidence more fitting for an endocrinologist to be delivering? Was this not ‘expert opinion’ that should naturally required an ‘expert in endocrinology’ to deliver? This unnamed doctor was also the person who testified that there were no other babies on the unit receiving insulin during the period Baby F was on the unit. Clearly the Judge picked up the same discrepancy I did regarding Baby E because, when he appeared to specifically questioned this evidence from the bench, she corrected her testimony to say that she was not referring to Baby F’s entire stay, only specifically to insulin prescriptions written on the dates of August 4 and 5. This is at best deliberately misleading, and at worst a lie - as Baby E was still on the unit until his death at 1:24am on August 4. Insulin already ordered and delivered for Baby E, which as we have already seen would have been labelled with the same surname as Baby F, would have still been in the fridges of the neonatal unit during much of August 4 and possibly into August 5. We have already seen several instances of similar misleading evidence put before the jury, and while in each case the evidence appears to sit right at the border of truth and deception, it is couched in such a way as to give the jury and mainstream media a perfect soundbite. People tend towards remembering the soundbite. They rarely realise the omission, and almost never recall the correction.
Dr Gibbs also testified that he had concluded in hindsight on August 5 that a bolus of insulin must have been administered during the night, but that he had not thought of it during the phone call with Dr Harkness. The phone call between Dr Harkness and Dr Gibbs is described variously as having happened at 1:30am and 3:30am and later as having been written up at 2:30am. It is possible that this was two phone calls and the two got confused during testimony. It is also possible that in being transcribed from the verbal testimony that the two times got crossed over or were a typo. I have chosen to stick with the earlier 1:30am time because events such as the follow-up blood glucose tests and prescription of 10% Dextrose that were prospectively discussed during the phone call were noted as having occurred at, for example, 1:54am. In order for them to have occurred after the plan to undertake them was conceived, the call had to have occurred prior to 1:54am. Later testimony that he wrote the clinical note at 2:30am also supports that the call must have occurred at 1:30am.
Another interesting piece of evidence that arose during testimony regarding Baby F was that the unnamed nurse admitted that she breached what would be normal and legal protocol in a healthcare setting - that at some point during the day shift she co-signed as a witness, attesting to administration of medication that was documented as having occurred during the following night shift at 2am. To show you that I was not the only person who heard her admit to co-signing medical records to say she had witnessed medication administration that she was not on-shift or even physically present on the unit to have seen, here’s how The Chester Standard described her overt admission:
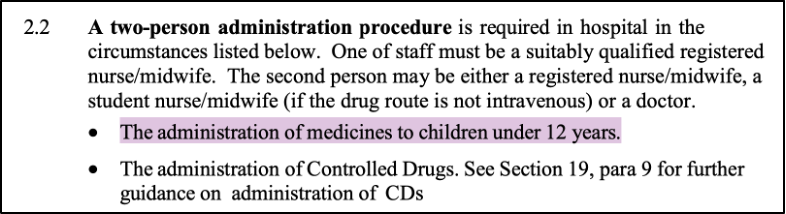
Below is an extract from the hospital policy on administration of medications:
I also looked at policies from other hospitals, finding that it is common practice that all administrations (i) to persons under the age of 12; or (ii) where the medication requires the calculation of a weight-based or volume-based dose, requires the presence of two members of clinical staff during the entire procedure (examples taken from: here and here):
The lack of a witness creates potential for a number of issues. Anyone reviewing these medication administration records will assume, based on the fact that a witness co-signed for administration, that per hospital policy the co-signer fully witnessed correct dosage preparation, drawing up and administration to the right patient. This assumption is patently flawed where the witness who co-signed for administration was a member of staff on the preceding day shift, and who had not been present on the ward for almost 6 hours. In such circumstances it is entirely possible, and difficult for the administering nurse to disprove, that the wrong medication or dosage or no medication at all was administered to Baby F. It is also possible that a harried, busy or distracted nurse could have given a medication still present in the ward supply for “Baby 1 [Surname]” to “Baby 2 [Surname]” - that is, the insulin that was almost certainly still present on the unit for Baby E to his twin brother, Baby F.
There was no evidence to suggest that Lucy Letby had anything at all to do with this ‘un-witnessed’ but ‘co-signed as witnessed’ medication administration.
A possibly interesting omission in the prosecution case that the defence does not appear to have picked up on is the absence of evidence regarding whether Baby E’s insulin was returned to the hospital pharmacy for re-distribution or disposal. In most hospitals, unused medications either made up or ordered specific to a patient and having a short expiry period would normally be returned to the pharmacy and recorded in a register prior to disposal. Had there been less insulin returned to pharmacy than expected the prosecution would assuredly have demonstrated this to the jury as it would have been a key piece of evidence proving that insulin was missing and that missing insulin was likely the source of Baby F’s alleged poisoning. That the prosecution did not present such information during the trial suggests either: (a) that they entirely missed collecting this evidence; (b) that the hospital pharmacy at CoCH did not record it; (c) that the prosecution knew that all the insulin was returned to pharmacy and was therefore accounted for but did not make the evidence available to the defence in discovery; or (d) that defence counsel failed to recognise the importance of this information and therefore failed Lucy by not drawing attention to it.
Another key issue that some may have missed and that it appeared Ben Myers KC got, but didn’t appear to develop, was the fact that there were two different TPN bags administered to Baby F during August 5. The first was started at 12:25am, and the second was started after the new long line had been inserted at 12:00pm. Ben Meyers KC questioned the doctors and nurses regarding the fact that it as standard infection control protocol to dispose of and replace the entire long line and any medications or TPN connected to it when the line was replaced. Professor Hindmarsh’s evidence was that the insulin must have been in the TPN because Baby F became hypoglycaemic after the TPN was replaced at 12:25am and “the [hypoglycaemia] issue persisted right through the day until the conclusion of the TPN bag at 6:55pm and the evidence he led in the form of a table suggests that it was the same (a single bag) TPN all day. Under cross examination Professor Hindmarsh acknowledged the existence of the second TPN bag, and that tests done at 5:56pm after the second bag had been hung would tell the court nothing about the level of insulin in the first bad at 12:35 am that morning. Professor Hindmarsh pointed to the paradox that existed in that Baby F’s blood glucose began to rise after his glucose infusions were ceased. This paradox might be explained by the effect of gluconeogenesis - in that Baby F’s liver may have finally been capable of forming glucose in the absence of parenteral inputs. It was also his evidence that the only explanation was that there had to be insulin in the TPN bag.
In any event there are legitimate reasons why an elevated insulin level might be seen absent a comparable c-peptide elevation. The simplest is that the laboratory analyst used the wrong test. Professor Vincent Marks, a Doctor of Medicine, Clinical Scientist and recognised expert on matters pertaining to insulin also points to the fact that doctors have all-too-readily accepted that simultaneous high insulin/low c-peptide means exogenous insulin administration, and potentially murder or attempted poisoning, even where there is absolutely no evidence that this is the case (here). Other examples in Prof. Marks paper include the use of samples that were too haemolysed and the mis-application of tests designed for serum or plasma to identify insulin and c-peptide in urine.
A final but important factor that should not have been ignored is that Dr Harkness accepted that the two primary problems he was treating Baby F for on August 5 were hypoglycaemia and tachycardia. Poor glucose control (hypoglycaemia) and alterations to cardiac rate (tachycardia) and output are known to occur together in neonates as a result of bacterial sepsis - and they occur as a result of bacterial endotoxins (here, here, here and here). This is a key factor that Dewi Evans, Professor Hindmarsh, Dr Harkness and the doctors at CoCH appeared, even while they acknowledge treating the neonate for ‘suspected sepsis’, to completely overlook in their race to accuse Lucy Letby of poisoning Baby F.
Even as each doctor distracted the jury away from the signs and symptoms that led to each neonate’s demise. And even as each doctor promotes the idea that these neonates were ‘doing well’ and denies that infection is an issue. Their own evidence demonstrates that every baby that passed through their unit, the ones that Lucy Letby stood accused of harming and others that were not mentioned in the trial, were all having issues with sepsis. Sepsis, not Lucy, was the common element in every baby’s demise.
The next article in our Lucy Letby Trial Series can be found here.
*********
The Law Health and Technology substack is entirely reader-funded. Many of the recent articles take a week or more to investigate and document. This is time not funded by an employer. Please consider becoming a paid subscriber to enable me to continue this work.
**********













I'd have thought that 'prewitnessing' an injection to be a very serious breach of safety protocols. It is unlikely this was a 'one off' and suggests tolerance of poor adherence to due process in the unit. A huge risk factor for poor outcomes in this very complex and technically demanding speciality.
The number of interventions tell me baby not doing well at all. One wonders how such a frail little human can even survive such an endocrine rollercoaster. It could be the way you are presenting it but I don't get a sense of competence. I could be more specific but too late today. I feel sad for the babies & Lucy.